Reflections
Your Bishop Score
Rates of induction have more than doubled in the past two decades. However, risk factors related to induction are also increasing to both mom and baby.
The Bishop score is the most commonly used method to assess the readiness of the cervix for induction. However, it was created without modern statistical methods.
The Bishop score, created in 1964, assesses the dilation, effacement, consistency and position of the cervix as well as the station of the baby. Each item is then given a score of zero to three and totaled up. If the score is an eight or higher, the cervix is favorable and induction is more likely to succeed. When the score is less than eight, there is a higher risk for complications and are more likely to have interventions to augment birth.
Here is a reference page that can be used to determine a Bishop score .
If a cervix is favorable, induction is likely to result in vaginal delivery, and any method of induction tends to work well. This includes any at home, natural methods that may be tried. If a cervix is considered to be unfavorable, no method is highly effective for induction. The cervix must “ripen” more so that it becomes favorable.
The risks of being induced vary depending on the method of induction, but the biggest risk is that induction will fail. In 25% of cases, induction is not successful. This may mean birth lasts longer than it would have without having an induction. This may ultimately lead to a c-section which can be physically taxing and emotionally draining for both mom and dad. It can also put the baby in distress.
If induction ends up being the right choice for your family you can still have a vaginal birth. Take a childbirth class to understand all the risks and benefits of various procedures. Then gather a supportive birth team-dads and doulas work great together. Believe in yourself. Believe in the process.
Mindfulness
Mindfulness is the ability to be fully present, aware of where we are and what we’re doing, and not overly reactive or overwhelmed by what’s going on around us.
Mindfulness is a quality that everyone already possesses, it’s not something you have to conjure up, you just have to learn how to access it.
When we’re mindful, we reduce stress, enhance performance, gain insight and awareness through observing our own mind, and increase our attention to others’ well-being.
Make listening to music, dancing, and singing a regular part of your pregnancy. It helps tune both mom and baby’s bodies. Music has been shown to reduce anxiety, heart rate, and respiratory rate. It also decreases stress hormone levels, boosts natural opiates, relaxes birthing women, and has beneficial effects on the physiology and behavior of the newborn, including contributing positively to weight gain in both normal-weight and premature babies.
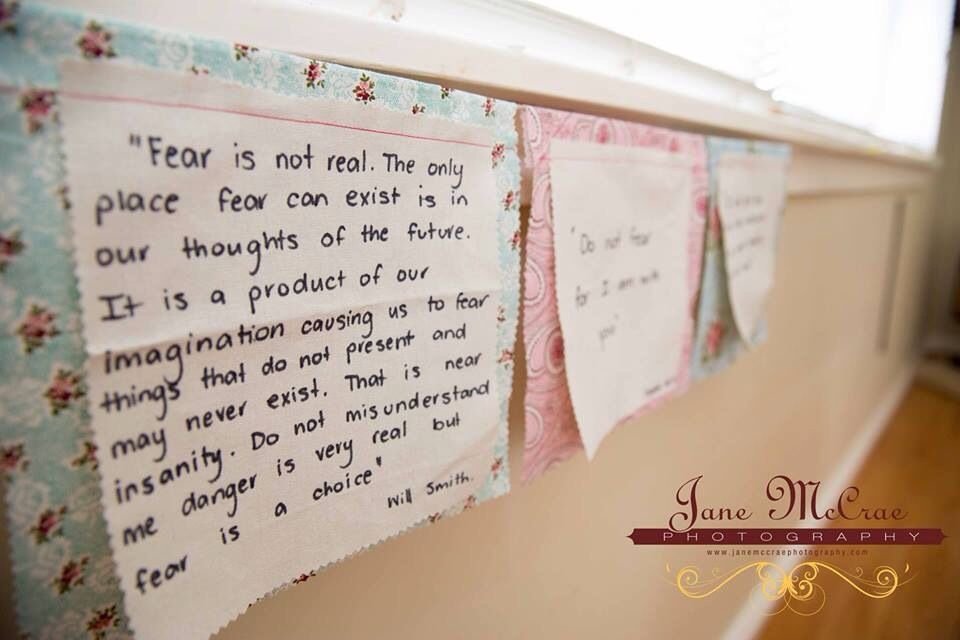
Take advantage of your emotional porousness. Use birth affirmations regularly during your entire pregnancy to help you program your body and mind for optimal birth. You may be surprised at your mind body connection.
Put affirmations all around your environment—your refrigerator, bathroom mirror, Bible, journal, and your phone/tablet lock screens—to remind you of your birthing power. Say them out loud or in your head regularly. Write them down repeatedly. Let the power of your emotions and thoughts do its magic with your body. Stay positive!
Studies have shown mindfulness training addresses fear, anxieties, and comfort level during childbirth can improve women’s childbirth experiences and reduce their depression symptoms during pregnancy and the early postpartum period.
One author of a study, Larissa G. Duncan, says, “A mindfulness approach offers the possibility of decreasing the need for these medications and can reach women who may not know they are at risk for perinatal depression or can’t access mental health services,” Duncan says.
Nancy Bardacke, another author of the study, believes, “The encouraging results of this small study point to the possibility that mindfulness skills can transform the way expectant parents prepare for this profound life change. In addition to supporting moms and babies, we may also be benefiting fathers, who are themselves experiencing the birth of their child and becoming parents. While more research is clearly needed, the larger public health implications of this work are motivating.”
Stay positive even when life seems to have fallen apart *ahem COVID*. Practice your mindful connection, visualize your perfect birth and lets make it happen.
Delayed Cord Clamping
Approximately 30% of the baby’s blood remains in the placenta and cord at birth; immediately shutting off this source can deprive him of 60% of the red blood cells. This placental blood supply carries 40 to 50 mg of iron, helping prevent anemia. For this reason, the World Health Organization recommends late cord clamping at least one to three minutes after birth. Most home birth midwives, however, do not clamp the cord until it stops pulsing (typically at least 3 to 5 minutes) allowing the maximum amount of the baby’s own blood supply from the placenta to enter the body.
Can delayed cord clamping cause any problems? In the past it was hypothesized that all that extra blood could increase physiologic jaundice in the newborn, but time has not shown this is true and it is no longer considered an issue.

Concerns about delayed cord clamping also surround the mother. It has been implied that delayed cord clamping may lead to an increase in postpartum hemorrhage.
However, there is no statistical evidence proving that delayed cord clamping results in an increase in blood loss. There is also no significant difference regarding blood loss greater than 500ml between early and delayed cord clamping.
Are there instances when the cord should be clamped immediately? Yes, but they are rare. One possible scenario would be a very tight cord preventing the baby from being born. Even when babies need help breathing, experts believe it best to keep the cord intact so the baby is continuing to receive oxygenated blood from the placenta. Keeping the lifeline connected can only help as baby makes the transition to the outside world.
If you are planning a hospital birth, you may want to discuss with your doctor or midwife how long the cord may be left intact for your baby. If you are planning out of hospital birth, your midwife can explain what her practice is and why she holds that position.
Nausea During Pregnancy
Nausea and vomiting is very common in early pregnancy. It can affect you at any time of the day or night, and some women feel sick all day long.
Nausea may be unpleasant, and for some women it can significantly affect their day-to-day life. Usually it will clear up by weeks 16 to 20 of your pregnancy.

When you get pregnant, your hormones shift to support the pregnancy. For most women, it is this surge in hormones that causes nausea and vomiting. When your placenta takes over hormone production in the second trimester is when you will find relief.
If your morning sickness isn’t too bad, your midwife may initially recommend you try some lifestyle changes:
- get plenty of rest
- avoid foods or smells that make you feel sick
- eat something like dry toast before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones
- drink plenty of fluids, such as coconut water or a liquid IV drink
- eat foods or drinks containing ginger
- try acupressure – there’s some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
- try getting more vitamin B6 through whole food sources. Some times a deficiency causes nausea.
- if you have tried “all the things” don’t be afraid to ask your care provider for a prescription medicine. This may be your best option to curb nausea.
Few people would disagree that nausea is one of the worst parts of pregnancy, as it can keep you from enjoying this special time and severely limit your ability to participate in everyday life. Thankfully, for most women, it’s short-lived and eases by the second trimester.
Postpartum Meals
The transition from pregnancy to postpartum is enormous — especially because it involves a newborn baby, making milk, and almost nonexistent sleep. Add that to the fact that you’re recovering from just having birthed a baby and your world is full.
It is a good idea to plan nourishing meals for the first few weeks after baby is born. But what?? You may not have a large freezer and relying on a meal train may not be feasable – especially if you have allergies.

To support this shift, it’s important to focus on warming, easily digestible, mineral-rich foods to promote healing and provide sustained energy. Think properly-prepared grains, cooked veggies, nourishing fats, and ferments.
When I was pregnant I froze homemade pancakes, soup, lactation cookies, burritos, smoothies, and giant meatballs. They reheated quickly and for the most part could be eaten one handed if I was holding my new squish.
Whatever meals you choose make sure they are foods that support breastfeeding and promote healing. Eating healthy is even more important postpartum! You are recovering physically, while also providing nourishment for your baby by breastfeeding. This double strain on your body requires a lot of fuel!
Your job in the “fourth trimester” is to nourish your baby, eat a balanced diet and sleep as much as you can. Fortunately, adequate sleep and a healthy diet will help you lose some weight. But this is not the time to try some type of postpartum weight-loss diet or restrict calories, which could cause your milk supply to drop if you’re breastfeeding. And, whether you’re breastfeeding or not, calorie restriction combined with a lack of sleep is a recipe for cravings, overeating and binge eating.
Your body just completed an amazing feat and really needs time and attention to heal, and that often gets brushed over. Plus the sleep deprivation, the laundry, the dishes can all wait. Providing your body with good nutrition, gentle movement and your brain and heart with patience and attention can help you feel more at peace. Be really kind to yourself, Mama! And sleep when the baby sleeps.
Postpartum Planning
While you are pregnant and planning for a new baby, make sure that creating a postpartum plan is at the top of your priority list!
Many expectant parents spend most of their preparation time planning for childbirth and getting the nursery ready, but few parents really “get” the need to prepare for postpartum recovery.

You often have very little control over how your pregnancy, birth, and early weeks postpartum will go. You may have an easy birth and recovery, or you may have lots of challenges to overcome.
Most new parents do face some challenges, especially fatigue. When you plan ahead and have help set up, you have at least some control over how your recovery will go.
Having a postpartum plan is like having an insurance policy. If you have it, you may not need it, but if you don’t have it, you may really need it (but it will be too late to create one.) At that point, you will need to scramble for help. Please do not wing it!